While discussing risk factors for aspiration pneumonia with a group of SLP graduate students, I noticed a trend in the conversation. The more questions they asked, the fewer answers I could give them. It wasn’t that the answers existed and I didn’t know them; instead, these astute students wanted to know where to find information that explained the sequence of events that occur when food or liquid enters the lungs and eventually develops into pneumonia. They wanted the article or textbook that would show something like, “Food or liquids enter the airway and travel to the gravity-dependent lobe of the lung, enters into the alveoli where an infection develops, and then an immune response begins.” Given the level of certainty with which these students were discussing how they perceived aspiration pneumonia development, they were pretty surprised when I informed them that no such reference existed! Here’s the deal: when you search the literature in dysphagia research, pulmonology, and even microbiology, you end up down a winding road with many divergent and often confusing paths with few answers and an ever-growing number of questions. Given the heavy toll that respiratory illnesses such as aspiration pneumonia have on those with ID, let’s take a deeper dive into some of these very questions.

“Pneumonia is an opportunistic disease developing in persons who are already seriously ill frail, or debilitated” – Barlett, 1975’
Defining aspiration pneumonia: Simple enough, right?
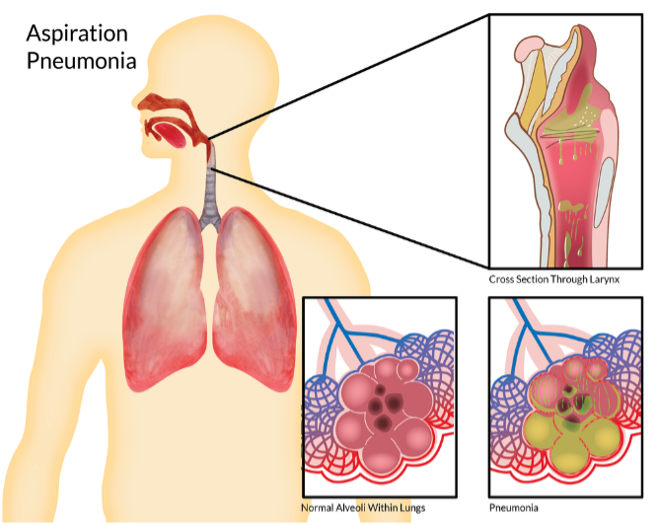
Nope! When a patient is diagnosed with aspiration pneumonia, most clinicians may associate the diagnosis with the aspiration of food or liquids. However, “aspiration pneumonia” is a vague diagnosis that may result from a pulmonary infection, gastroesophageal reflux, or prandial aspiration [1]. Numerous respiratory syndromes are often labeled as “aspiration pneumonia.” These include community-acquired pneumonia, hospital-associated pneumonia, ventilator-associated pneumonia, and pneumonitis. At its most rudimentary level, a diagnosis of aspiration pneumonia merely refers to a pulmonary infection resulting from colonized foreign matter entering the lungs. Because of this lack of terminology specificity, some medical professionals now advocate for outright elimination of the term “aspiration pneumonia” because it can be misleading [2].
“Aspiration is necessary but not sufficient to cause pneumonia”– Langmore et al., 1998
Diagnosing aspiration pneumonia: The chest X-ray, right?
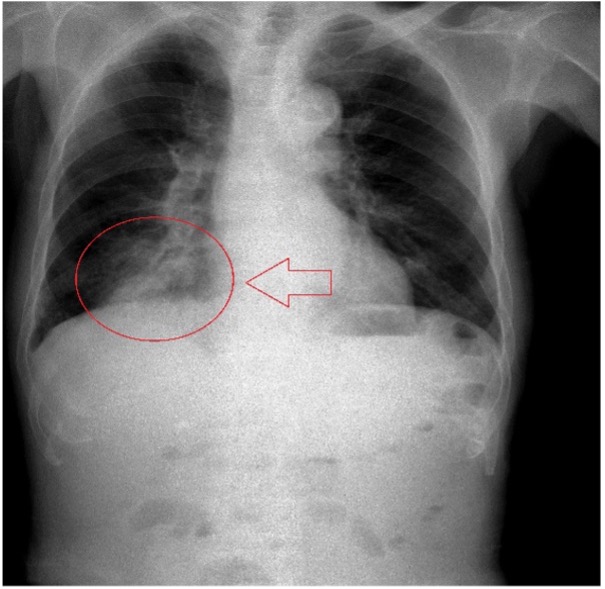
Not exactly! While radiographic imaging is necessary for a comprehensive diagnosis of pulmonary infection [3], the chest X-ray cannot definitively diagnose aspiration pneumonia. About two-fifths of those hospitalized for pneumonia (41.2%) are diagnosed based on a CT scan, about two-thirds involve a chest X-ray (65.1%), and one-third involve a pulmonary function test (33.7%). In 2014, the CDC reported that 75% of inpatient hospitalizations for pneumonia were diagnosed based on bacteriology and microbiology testing. Such testing is a more reliable diagnosis for pneumonia based on detecting actual pathogenic agents in the lung parenchyma. Unfortunately, we clinicians often only have access to and thus rely on a chest X-ray alone. What’s important to know is that the ability to diagnose pneumonia from a chest X-ray has a sensitivity of 69.0 and a specificity of 77.8. In other words, a radiologist correctly interprets pneumonia from a chest X-ray 69% of the time and correctly eliminates pneumonia 77% of the time! Based on this diagnostic sensitivity, reliance on X-ray findings alone is discouraged [4]. When reading X-ray reports, most clinicians traditionally consider lower lobe infiltrates indicative of aspiration pneumonia. However, in a study examining a group of patients with documented aspiration via a MBS exam, 68% presented with bronchopneumonia, while only 13% were identified with lower lobe pneumonia [5]. This begs the question: can a chest X-ray accurately diagnose aspiration pneumonia? At the moment, there is no simple answer, as there is convincing evidence that a chest X-ray alone is not enough to allow for the diagnosis of aspiration pneumonia a good part of the time. When we ask, where does aspiration pneumonia appear on a chest x-ray? Here again, there is conflicting information. Have we been searching in all the wrong places? Perhaps. See what I mean: the answers are evasive, and the questions are many!
Tying it all together: Embrace a new perspective.
In summary, pneumonia is often considered a linear process where changes in a few key factors (aspiration, virulence of the pathogen, and strength of the host defense) cause a predictable inflammatory response in the lungs. But in actuality, pneumonia occurs abruptly and unpredictably from the complex, adaptive system of the respiratory microbiome. Unlike linear systems, these complex and adaptive systems can’t be reduced to such a simple model. The discovery of the lung microbiome and the recognition that the lungs are a dynamic ecosystem has changed our understanding of pneumonia development. The current literature now points us towards issues of balance between bacteria within the oral, pharyngeal, and gut biomes and the pulmonary reactions of the host. It may be the presence of certain bacteria in the oral cavity and gut that cause inflammation and infection in the lungs. Or, it may be the host’s inability to respond to the bacteria in the lungs that ultimately leads to infection. Whichever the case, many questions remain unanswered. Why do some people develop pneumonia due to prandial aspiration and others don’t? The development of pneumonia depends on multiple factors that often defy the explanation. However, it’s not as simple as “aspiration occurred on a swallow study so that aspiration pneumonia will develop.” As such, we must shift our focus from the narrow view of the throat (i.e., aspiration vs. no aspiration) to the broader characteristics of the whole person to make better decisions that can help mitigate aspiration pneumonia risks in those we serve.
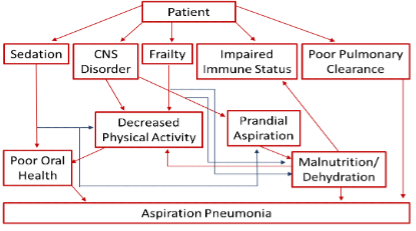
“There is not a simple and obvious relationship between primary aspiration and pneumonia”; Aspiration pneumonia flowchart– Komyia 2013.
The scoop of the week references
- DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care. 2015;30(1):40-48.
- Ferguson J, Ravert, B., Gailey, M. Aspiration: /aspə’ā SH(ə)n/: Noun: An ambiguous term used for a diagnosis of uncertainty. Topics in Pulmonary Medicine. 2018;25(5):177-183.
- Mandell LA, Niederman MS. Aspiration Pneumonia. N Engl J Med. 2019;380(7):651-663.
- Raghavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Critical Care Medicine. 2011;39(4):818-826.
- Komiya K, Ishii H, Umeki K, et al. Computed tomography findings of aspiration pneumonia in 53 patients. Geriatr Gerontol Int. 2013;13(3):580-585.